
If you are interested in becoming a living kidney donor and are in good health, here are some steps you can take. More details
The renal unit was born from an extremely humble beginning. It was conceived in ‘Fagin’s den’ on the 4th floor of The Charitable Infirmary, Jervis Street, which was previously the junior doctor’s residence.
The founding fathers of the department were Dr. A.P. Barry, MD, MAO, FRCOG, consultant gynaecologist; Gerard Doyle, MD, FRCPath, consultant pathologist; William F. O’Dwyer, MD, FRCPI, consultant senior physician with an interest in renal medicine; Mr. Anthony Walsh, FRCSI, consultant urologist, and Dr. Joseph A. Woodcock, FFA, consultant anaesthetist.
The need then was to try to save the lives of young women who had developed complete acute renal failure due to the complications of pregnancy. The founding fathers responded and purchased a Kolff Twin‐Coil Artificial Kidney, the first in the country. Four members of the team were trained in the techniques of dialysis in Leeds. So, the first dialysis began in May 1958.
Figure 1. Kolff Twin-Coil Artificial Kidney

In the first year most of the dialyses were done at night, each session taking approximately nine hours. Only patients who had acute renal failure were treated. In January 1963, Dr. Michael Carmody was appointed as the first medical intern to the Renal Unit. Nurses became increasingly involved in the management of haemodialysis. They quickly adapted to a rapid, rising tide of technology, applied biochemistry and complex patient care. All this happened at a time when the dialysis unit in Jervis Street Hospital with its two artificial kidneys was the only facility in the Republic for the treatment of renal failure.
Jervis Street Hospital commenced its programme for regular dialysis therapy in November 1964, as treatment was extended and offered to patients with irreversible renal failure, leading to an expanding population of patients, whose lives were being maintained by the provision of regular haemodialysis therapy. The criteria for selection of patients for regular haemodialysis were that they should:

Figure 2 Prof. Joseph Walshe, Sr. Mary Doyle, Dr. Yvonne O’Meara, and Dr. Alan Byrne with a patient in St. Martin’s Haemodialysis Unit, Jervis St.
The next momentous occasion in the unit was on the night of the 31st January 1964 when the first cadaveric kidney transplant was performed in Jervis Street Hospital. The elation which followed was short-lived as the recipient died shortly afterwards. Three more cadaveric renal transplants were performed that year with the same outcome. No transplant was performed in 1965 and only one in 1966.

Figure 3. The Charitable Infirmary, Jervis Street 1718-1987.
The programme recommenced in 1967 with renewed enthusiasm since newer immunosuppressive agents had become available. For all future transplants azathioprine and prednisilone was the regime utilised. Tissue typing, which was introduced in the early 1970’s, became another major advance in the field of transplantation. The matching of donor and recipient called for transportation of kidneys on a wide geographical basis, as hospitals throughout Ireland soon became involved in providing donor kidneys, and the Irish Army helicopter service played a valuable role in collecting the donor organs.

Figure 4 Mr. Seán Hanson and staff-nurse Roisín Owens in St. Damien’s Ward, Jervis St.
The living related kidney donor transplant programme commenced in July 1972. Peter McLean, who had participated in the renal transplant programme from the outset, returned to the consultant staff of the hospital in 1968 after completing his training in the US and took on the responsibility of expanding the kidney transplant programme.
With the rapidly increasing workload, the staff was further expanded with the appointment of Mr. J. Seán Hanson as a full-time consultant transplant surgeon in 1975. Although the early years of transplantation were extremely stormy and results were poor, the programme increased in its scope and expertise to the point where success rates for recipients are comparable with the best figures worldwide.
By the end of the 1950’s the principles and techniques of the management of acute renal failure were well established. Little progress however had been made in dealing with end-stage renal failure, the treatment of which called for frequent access to the circulation for an indefinite period of time, and there was no satisfactory technique for doing so. At this time almost every treatment required a fresh cannulation of an artery and vein and after some weeks many patients had no suitable vessels remaining, with devastating results. Because of the successes in dealing with acute renal failure, the unit was inundated with requests to treat end stage renal failure patients.
A major development occurred in Seattle in 1960 when Quinton, Dillard and Schribner reported on an exterior shunt composed of teflon and silastic which allowed repeated access to the vascular system for dialysis. This breakthrough was quickly adopted throughout the world and a new era in chronic haemodialysis began.

Figure 5. Schribner Shunt
In 1966, Cimino and Brescia described a new concept of access to the circulation using a surgically created arteriovenous fistula (AVF) in the forearm. The first AVF was created in Jervis St. by Professor P.G. Collins, assisted by Dr. Carmody on the 31st December 1966. Mr. Hanson, was largely responsible for the introduction of the AVF technique into Ireland and western Europe with the publication of a paper in the British Medical Journal in 1967. So stable were the constructed fistulae in the great majority of cases, that it led the way for expansion of the home dialysis programme, as the patients had no difficulty in needling themselves three times a week.
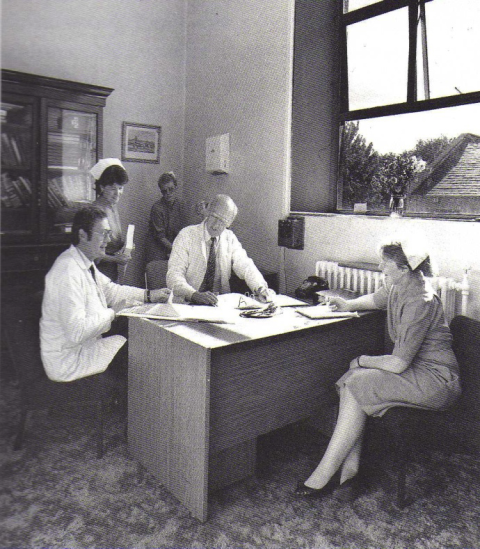
Figure 6. Dr. John Donohoe, Dr. Michael Carmody, Sr. Josephine Mc Manus, Sr. Bridget Hogan & Sr.
Maureen McNulty in Unit C
In the early days, many patients were underdialysed receiving treatment on only one day each week. Regular dialysis soon led to the obvious extension of the facility to the patient’s home. This reflected improved safety of the required technology and was of major benefit to patients who would otherwise have to commute long distances for hospital dialysis. In October 1970 the first patient commenced training for the home programme in the plaster room. The original criteria for acceptance onto the regular dialysis programme was exceptionally rigid and involved the acceptance of patients who would ultimately benefit from transplantation. The only exception to this selection criterion at the time was the placement of patients on home dialysis for which this mode of therapy was their final choice. In 1982, the development of the Continuous Ambulatory Peritoneal Programme (CAPD) offered patients an alternative modality of home dialysis treatment.
A hospital based regular dialysis programme continued to be the major form of renal replacement therapy within the unit in Jervis Street. The artificial kidney unit (St. Martin’s) opened on the 10th March 1979 with 9 dialysis stations, later to be increased to 11 stations, and was located on the first floor of the original maid’s home. St. Martin’s was full to capacity, working 24 hours a day, seven days a week, with approximately 70 patients maintained on thrice weekly treatments in 1987. Because the facility was worked to capacity, a backlog of patients had developed in a smaller dialysis facility, Unit C in St. Mary’s Hospital in the Phoenix Park, which had been originally designed as an acute dialysis setting.

Figure 7. Dr. Michael Carmody with Nurses Mona Campbell and Nuala Coyle, and Sister Maureen
Flemming in Unit C
Literature cited
Carmody, M (1987) The Department of Nephrology and the development of Kidney Transplantation.
In The Charitable Infirmary 1718‐1987: A farewell tribute.
Carmody, M. (2006) How the Specialty of Nephrology was Born. Irish Medical Times.
Hogan, B. (2006) Opening Address at 8th Annual INNA Conference. Beaumont Hospital, Dublin.
March 4th 2006.
By:
Ciara White, Renal Nursing Education Co‐ordinator, Beaumont Hospital.