
Lorem ipsum dolor sit amet, consectetur adipisicing elit, sed do eiusmod tempor incididunt. More details
Early prostate cancer can be treated in a number of ways. Both you and your doctor together will decide which treatment suits you best. It is common for you to be asked to make a decision about which treatment suits you best. In making your decision, your doctor and nurse will support and advise you.

The following treatment options are available:
Sometimes you may have fewer treatment choices than those listed. Many things can affect which treatment options are suitable for you. These include::
The stage and grade of your cancer
Your doctor will discuss your treatment options with you. If your prostate cancer is diagnosed at a later stage, call the Rapid Access Prostate nurses on 01 8528377 or the National Cancer Helpline on 1800 200 700. Click this link to dowload a copy of Understanding Prostate Cancer beyond the Prostate Gland. Or visit a Daffodil Centre.
Active surveillance: This is a treatment option for low-risk prostate cancer, which can be very slow growing and often does not cause symptoms or cause problems. Active surveillance aims to avoid or delay treatment if your cancer is likely to be slow to change and unlikely to threaten your health. It allows you to avoid the side-effects of treatment. It also aims to find cancers that change and start to behave more like fast-growing ones, and to offer treatment before the cancer spreads. During active surveillance you will be checked (monitored) with repeat blood tests and biopsies. If there is any sign of activity in your cancer, you will be offered treatment to cure the cancer. Active surveillance can carry on for many years if your cancer shows no signs of changing.

Radiotherapy: Radiotherapy is a treatment that uses X-rays to kill cancer cells. It can be given externally or internally. When given internally, it is called brachytherapy. When given externally, it is called external beam radiotherapy.
Brachytherapy: In this form of internal radiotherapy, radioactive seeds are placed in your prostate gland. They release radiation slowly over the following months. The seeds are very small, about the size of a grain of rice. The number of seeds implanted depends on the shape and size of your prostate gland. Not all men are suitable for brachytherapy.
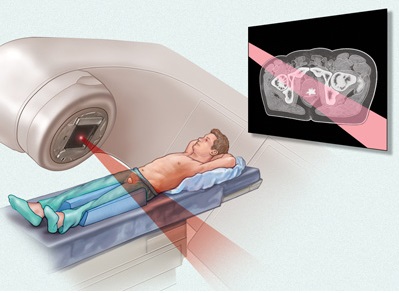
External beam radiotherapy: This uses high-energy X-ray beams to destroy the cancer cells. Radiotherapy can also be used together with hormone therapy, if needed. It is suitable for most men, although it may not be the best option if you have urinary symptoms.
Surgery: The operation to remove your entire prostate gland is called a radical prostatectomy. There are several ways of doing it. For example, traditional open surgery, keyhole surgery, and robotic keyhole surgery.
Watchful waiting: Prostate cancer often grows slowly and does not cause symptoms. For some men with early prostate cancer who have other health issues this may be a reasonable option. Watchful waiting is different from active surveillance. It involves PSA testing but no repeat biopsies. Also, it may suit you if your prostate cancer changed but you were not suitable for either surgery or radiotherapy.
Deciding on treatment
At this time you may be anxious about what is going to happen next. Do not be afraid to ask your doctor or nurse. They will discuss your treatment options with you. Many men find making a decision about which treatment they should have difficult. Do remember that your doctor will tell you if one treatment is better than another at getting rid of your cancer. But often they cannot because the treatment options are all thought to be equally good at treating early prostate cancer.
Very often there is no rush to make up your mind about which treatment to have. It is good to take time to talk to a urologist and a radiation oncologist before you make up your mind. Taking time to talk things through with doctors and nurses, family and friends can help you to reach the right decision for you. You will need to think about what the treatment involves for you, the impact on work or daily activities, and which side-effects you feel you can live with.
Asking questions: Do ask your doctor and nurse as many questions as you like, no matter how small or trivial you think they are. All questions are important. If you forget to ask a question or would like more explanations, call the Rapid Access Prostate nurses on 01-8528377. National Cancer Helpline on 1800 200 700 and talk to a specialist nurse or visit a Daffodil Centre.

Surgeon/Urologist
A doctor who specialises in surgery to the prostate, kidneys and bladder.
Radiation oncologist
A doctor who specialises in treating cancer patients using radiotherapy.
Dr Brian O’Neill
Liaison oncology nurse or clinical nurse specialist
A specially trained nurse who works with men with prostate cancer. She or he gives information and reassurance to you and your family from diagnosis and throughout treatment.
Teresa Doyle CNS Oncology
Prostate coordinators
Sara White
Clodagh Sharpe
Eimear Dunne
Radiation Advanced Nurse Practitioner
Clare Farrell
Urology Nurse Specialist
Rachael Swords
Radiation therapist
A radiotherapist who specialises in giving radiotherapy and advice to cancer patients.
Dr. Brian O’Neill
Medical Oncologist
An oncologist specialises in giving chemotherapy and advice to cancer patients
Prof Grogan
Physiotherapist
A therapist who treats injury or illness. You may be taught pelvic floor exercises by a physiotherapist if you have surgery for prostate cancer.
Medical social worker
A person specially trained to help you and your family with all your social issues and practical needs. They are skilled at giving emotional support. They can also give advice on benefits, entitlements and services available to you when you go home.
Counselor
A person specially trained to give you emotional support and advice when you find it difficult to come to terms with your illness. The Irish Cancer Society provides a counselling service. For details, call the National Cancer Helpline on 1800 200 700. ARC Services. Gary Kelly. MAC. Daffodil Centre.